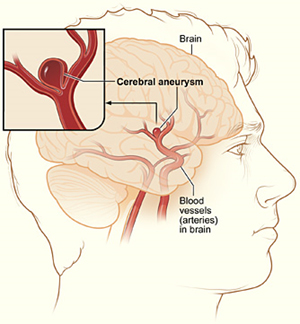
A cerebral aneurysm is like a blister on a blood vessel. As with a blister on the skin, the blister on the blood vessel is made up of thinner and weaker material—bulging and at risk of breaking. A cerebral aneurysm is an “outpouch,„ or ballooning, of a weakened blood vessel wall in the brain. The ballooned segment disrupts normal blood flow through the vessel and can lead to blood clots or rupture of the aneurysm. The larger the ballooned section becomes, the greater the risk that it will burst and then cause bleeding into the brain. Many aneurysms are found at the junction of the large arteries at the base of the brain, in an area referred to as the Circle of Willis.
There are three types of cerebral aneurysms: saccular/bifurcation, sidewall and fusiform:
Aneurysms are also classified by size:
An arteriovenous fistula (AVF) in the brain is an abnormal connection between an artery and a vein found in the tissue that covers the brain and spinal cord. Unlike an arteriovenous malformation (AVM)—which patients are born with—an AVF is an acquired lesion, or developed later in life. The two main kinds of AVFs are dural AVFs (dAVF) and carotid-cavernous fistulas (CCF).
Dural Arteriovenous Fistula (dAVF): One of the layers of the membranes that cover the brain is called the dura mater. An abnormal connection between blood vessels that involve this covering is called a dural fistula, which can occur in any part of the brain covering. A dAVF often involves the transverse-sigmoid sinus (behind the ear) and sagittal sinus. Patient reports of hearing a continuous “swooshing„ noise that coincides with their heartbeat (called a bruit) are common. Other symptoms include pain behind the ear, headaches and neck pain.
Cavernous Carotid Fistula (CCF): CCFs occur behind the eye and almost always cause visual symptoms due to diversion of blood flow to the eye and consequent increase in eye pressure. Symptoms can include eye swelling, decreased visual acuity, redness of the eye, congestion of the eye, droopy eyelid and pain of the eye. Patients also might report hearing a “swooshing„ noise.
There are two categories of CCFs: direct and indirect. A direct CCF has connections between the carotid artery and the veins of the cavernous sinus, usually due to trauma or ruptured aneurysm. An indirect CCF is an abnormal connection in which small arterial branches supply the veins and usually occurs spontaneously. Both types of CCFs threaten vision as well as eye movement, and both can result in major stroke.
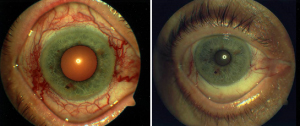
Picture of eye before and after treatment of carotid cavernous fistula with Onyx embolization. Note how the redness of the eye is much improved.
Endovascular embolization is used to treat dAVF and CCF. Embolization is a minimally invasive endovascular technique that consists of placing a microcatheter from the femoral artery inside the fistula (abnormal connection) and injecting an embolic agent under x-ray guidance to occlude, or fill, the irregular blood vessels. This treatment re-directs blood flow to the normal, healthy part of the brain and seals off the abnormal connection stealing blood flow. For those patients who experience a “swooshing„ noise, the sealing off of this fistula will provide immediate relief from this noise with successful embolization.
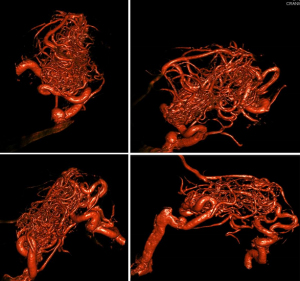
An arteriovenous malformation (AVM) in the brain is a complex tangle of thin-walled blood vessels—an abnormal connection between arteries and veins within the tissue of the brain or spinal cord—that can break more easily than normal, healthy vessels.
Unlike an aneurysm or stenosis, which can occur and be cured at any point in a person’s life, AVMs are usually congenital, or part of the brain from birth.
Symptoms of an arteriovenous malformation can vary depending on the location of the lesion and can include:
An arteriovenous malformation contains abnormal, weakened blood vessels that direct blood flow away from normal brain tissue.
These abnormal blood vessels dilate, or get bigger, over time and can eventually rupture from the high pressure of blood flow from the arteries to the veins. The chance of having an intracranial hemorrhage (ICH) from an AVM is 1-3% per year.
There is a 10-15% risk of death from the initial bleed and a 25-30% risk of permanent disability from the brain injury.
Most AVM’s are diagnosed after a patient shows symptoms, but sometimes are found incidentally. The most common testing approaches include:
Brain AVMs must be treated delicately and many patients are treated using a combination of therapies.
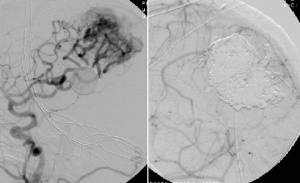
Imaging of an AVM before (left) and after (right) embolization treatment.
AVMs are a neurovascular disorder that require a neurosurgeon to have expertise in all three areas of treatment: conventional surgery, endovascular surgery and radiosurgery. In general, treatment of an AVM is recommended if it has bled, if it is an area of the brain that can be easily treated and is not too large in eloquent areas of the brain serving vital functions of the body.
A multidisciplinary team must consider the neuroimaging, anatomical, functional and dynamic information of an AVM patient before formulating a strategic treatment plan.
Creating the plan involves weighing the relative risks and benefits of a conservative approach vs. surgery vs. radiosurgery vs. embolization (deliberate blocking of a blood vessel or part of a blood vessel) or a combination of these therapies.
Treatment options include:
Of these options, the practice of embolization has advanced the treatment of AVMs most notably in recent years.
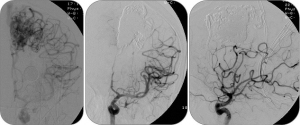
Imaging of AVM embolization treatment with Onyx.
Embolization is a minimally invasive endovascular technique that consists of placing a microcatheter inside the AVM and injecting an embolic agent under x-ray guidance to occlude, or fill, the irregular blood vessels.
Craniotomy and AVM resection using microsurgery is a direct approach to remove the AVM and obtain cure. It is usually reserved for lesions located in more accessible areas of the brain.
Radiosurgery is another minimally invasive approach that involves aiming multiple narrow beams of highly focused radiation from different directions to converge directly at the AVM. The high dose of radiation concentrated only in the AVM and sparing the brain promotes a gradual occlusion of the AVM. This process will not cure the AVM immediately but rather over time the AVM “dies off.„
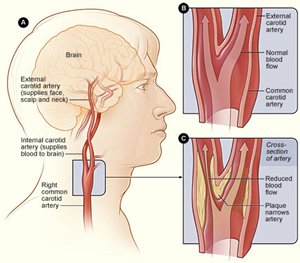
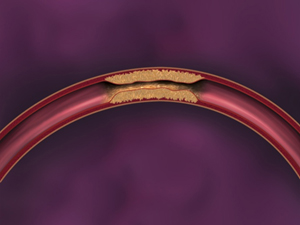
Carotid artery disease occurs when fatty deposits, called plaques, clog carotid arteries. The carotid arteries are a pair of blood vessels that deliver blood to the brain. Carotid artery stenosis is the narrowing or constriction of the carotid artery. It is possible to have stenosis of both carotid arteries. The buildup of plaques in these arteries blocks the blood supply to the brain and increases risk of stroke.
Because carotid artery disease develops slowly and often goes unnoticed, the first outward clue about the condition may be a stroke or transient ischemic attack (TIA), also called a ministroke.
Treatment of carotid artery disease usually involves a combination of lifestyle changes, medications and, in some cases, surgery or a stenting procedure.
Carotid artery disease is caused by a gradual build up of an atherosclerotic plaque, a process called atherosclerosis, that can cause the carotid arteries to become narrow and stiff and this can impair blood flow to the brain.
Risk factors are habits that increase chances of developing carotid artery disease. Some risk factors a person can change—modifiable risk factors—and others a person cannot change—non-modifiable risk factors.
Modifiable risk factors include:
Non-modifiable risk factors include:
The biggest complication related to carotid artery disease is a stroke. The most common ways a stroke can occur in this instance are via reduced blood flow (hemodynamic) resulting in a decrease of blood going to the brain and potentially progressing to carotid artery thrombosis (total occlusion). Another possibility is that the atherosclerotic plaque ruptures and small pieces block blood vessels downstream in the brain (embolus). This cuts off blood supply to that particular area of the brain resulting in a stroke.
Warning signs of stroke and TIA include:
Carotid artery disease may not always come with symptoms. A healthcare provider may diagnose the disease by listening to arteries with a stethoscope. They may also obtain information by asking questions about a patient’s family medical history, performing a physical exam and ordering further tests. Some of these tests may include:
The goal in treatment of carotid artery disease is to prevent strokes. Treatment options depend on the severity of narrowing of the blood vessels. Treatment options can include lifestyle changes, medications, surgery, and interventional procedures. Often times a combination of these is used in the management of carotid artery disease.
A cavernous malformation, or cavernoma, is a type of vascular malformation that consists of abnormally thin-walled blood vessels grouped together in the central nervous system (brain and spinal cord). These blood vessels are like little pockets containing blood at a low pressure. A cavernoma looks like a mulberry. Constant leaking of blood often causes symptoms. About 25-30% of people with cavernous malformations in the brain never have problems related to this low-pressure, intermittent bleeding.
There are three types of cavernous malformations:
People with cavernomas in the brain may have the following signs of bleeding, or cerebral hemorrhage:
People with cavernomas in the spinal cord may have the following signs of bleeding:
The main tests used to diagnose cavernomas include:
Possible treatment options available for patients who have a cavernoma include:
An intracerebral hemorrhage is a type of stroke and occurs when a blood vessel in the brain ruptures and leaks blood into the brain tissue. Leaking blood under pressure can damage brain cells. It usually occurs very suddenly without warning signs.
There are many causes of ICH including:
Symptoms are related to the location of the hemorrhage and the size of the bleed. Symptom onset is usually acute, a sudden onset. Common symptoms include:
The diagnosis is often done with imaging techniques like:
The different causes of hemorrhagic stroke often need to be worked up with a detailed medical history, physical exam, including assessment of stroke risk factors, blood pressure reading and neurological exam, as well as imaging of the brain and or spine.
An intracerebral hemorrhage is a medical emergency and treatment goals include stopping the initial bleeding and relieving the pressure in the head. In some cases, it may require open surgery to remove a blood clot or to place a drain in the head to decrease and monitor pressure inside the head. If an aneurysm or arteriovenous malformation are identified, an open or endovascular procedure may be required to repair the source of the blood leakage.
If a patient is on blood thinner medication, this will likely be discontinued and/or reversed to lower the risk of further bleeding.
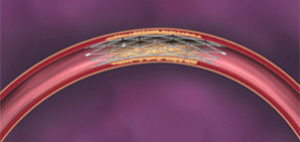
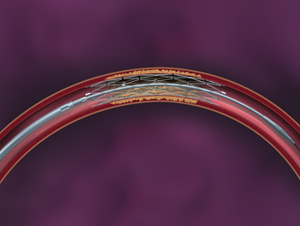
Intracranial Stenosis, or intracranial atherosclerotic disease (ICAD), is the narrowing or constriction of an artery inside the brain. Similar to carotid artery stenosis, intracranial stenosis is often caused by atherosclerosis—disease of the arteries characterized by the deposition of plaques of fatty material on their inner walls—and can lead to stroke.
The prevalence of ICAD varies among countries—and Asians, African Americans and Hispanics demonstrate higher rates of disease.
Hypertension, diabetes, smoking, high blood cholesterol and history of heart disease are all risk factors for ICAD.
The symptoms of intracranial stenosis vary depending on the location of the narrowed vessel:
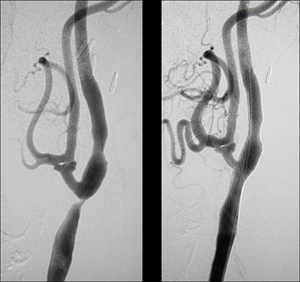
Medical management is currently the gold standard for the management of ICAD. Certain cases of recurrent symptoms, despite the best medical management, will require endovascular intervention. This has led neurosurgeons to the development of endovascular therapies, such as the minimally invasive stenting of vessels supplying blood to the brain inspired by the stents originally developed for use in the vessels supplying blood to the heart.
During the procedure, asmall stent made specifically for the brain is used to open up the blood vessel and reestablish blood flow.
Fibromuscular dysplasia (FMD) is a condition that causes narrowing (stenosis) and bulging of arteries of the body. These areas of narrowing and bulging occur right next to each other and often take on a “beaded„ looking appearance. Over time this can cause severe narrowing of the artery impairing blood perfusion to the area of the body that the artery supplies. It occurs most commonly in the renal arteries (kidneys) but can also occur in arteries of the brain, abdomen, arms and legs.
The cause of FMD is not known but there are several suggested theories. Some experts believe there is a genetic component due to FMD being diagnosed in multiple members of the same family, including twins. FMD is more common in women than men and some researchers believe that hormones play in role in development of FMD. This is supported by the knowledge that FMD tends to be diagnosed in women who are primarily premenopausal. Others suggest that tobacco use could cause abnormal development of the arteries supplying blood to the vessel wall and this could cause inadequate delivery of oxygen to the artery resulting in the changes noted.
The signs and symptoms of FMD depend on the organ the affected artery supplies.
When the carotid and vertebral arteries are affected, patients may experience dizziness, blurring or loss of vision, vertigo, neck pain, ringing or swooshing noises in the ear (bruit), TIA or stroke. FMD patients are also at an increased risk for intracranial aneurysms.
Diagnostic imaging is the only means for diagnosing FMD. CT angiography, MR angiography, carotid duplex ultrasound and cerebral angiography are all effective ways to diagnose FMD.
The imaging for the most common form of FMD, medial fibroplasias, shows arteries with a distinctive look of a “string of beads„ as opposed to a “straight tube-like appearance.„
There is no cure for FMD and there is not set a protocol or guidelines for treatment. Medical management is often the best form of treatment that can be offered and this is often done with measures to help increase and maximize blood flow and perfusion through the affected vessel.
Interventions can be offered but this is highly dependent on the vessel that is affected and the patient symptoms. Balloon angioplasty is most frequently used to open the carotid and renal arteries. Stents are not often used in treatment of FMD due to the disease being diffuse within the artery and often times not focal. It is typically recommended that people with FMD use some form of antiplatelet agent on a daily basis (usually aspirin or clopidogrel).
Head, neck and spine tumors can sometimes have a large number of blood vessels. This can make a surgical procedure to remove the tumor quite challenging. A pre-operative embolization is commonly recommended to decrease the blood flow going to the tumor and to decrease the blood loss during surgery for removal of the tumor.

Embolization is an endovascular approach used to block blood vessels that nourish a tumor. Liquid embolic agents are the most common materials used to block the blood vessels inside the tumor.
Types of tumors in these areas include:
Moyamoya disease is a rare, progressive cerebrovascular disorder caused by blocked arteries at the base of the brain (Circle of Willis). The word “moyamoya„ means “puff of smoke„ in Japanese and is a description of the look of the tangle of tiny vessels that are formed to compensate for the blockage. Moyamoya disease was first described in Japan in the 1960s and is most commonly seen in Japan and Asian countries. However, moyamoya has also been found in the United States, Europe, Australia and Africa. Moyamoya primarily affects children but it can also occur in adults.
The majority of individuals afflicted with moyamoya disease require some form of surgical intervention. Without this, many will suffer from multiple strokes and mental decline because of the progressive nature of the disease. Without treatment, moyamoya can be fatal if the result is an intracerebral hemorrhage.
Symptoms of moyamoya disease often include transient ischemic attacks (TIAs). Stroke is another possible symptom, which may include weakness of one side of the body or paralysis, visual changes, speech difficulties or seizures. Adults can more commonly experience a hemorrhagic stroke due to recurring blood clots in the affected brain vessels.
Diagnosis of this condition can include a review of symptoms and family and medical history, along with a neurological examination. It can also include specialized diagnostic testing to look more closely at underlying conditions, including:
There are several types of treatment options available for moyamoya disease. They are geared to restore blood flow to the brain by opening narrowed blood vessels or by bypassing blocked arteries. The goal of treatment is to reduce symptoms, improve blood flow and lower risk of serious complications, such as strokes, bleeding in the brain, known as intracerebral hemorrhages, or death. There are several types of revascularization surgeries to treat moyamoya disease. Below are the more common treatment options:
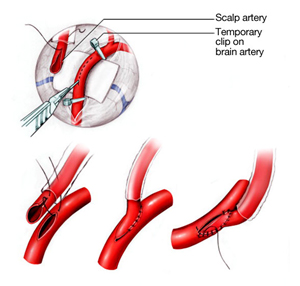
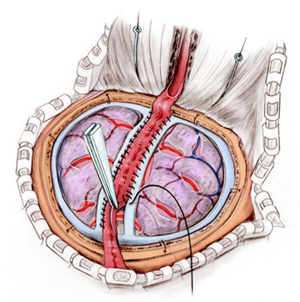
Direct revascularization procedures: In these procedures, a surgeon attaches a superficial scalp artery (superficial temporal artery or STA) to a brain artery (middle cerebral artery or MCA) by suturing one vessel to the other. This creates a new immediate path of blood flow to the brain. This approach can be more difficult for children due to the small size of the vessels.
Indirect revascularization procedures: One common approach is called encephaloduroarteriosynangiosis (EDAS). The surgeon using will dissect a superficial scalp artery over several inches. Then, using a temporary opening in the skull, will attach (or suture) this superficial artery to the surface of the brain. This allows the artery to help form new blood vessels to grow into the brain over time.
There are two types of strokes:
Ischemic stroke is the loss or lack of blood flow resulting in death of brain cells. Hemorrhagic stroke is a result of the leakage of blood outside of a blood vessel in the head, “bleeding in the brain.„
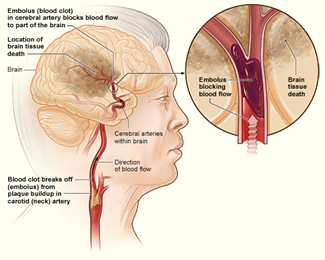
The illustration shows how an ischemic stroke can occur in the brain. If a blood clot breaks away from plaque buildup in a carotid (neck) artery, it can travel to and lodge in an artery in the brain. The clot can block blood flow to part of the brain, causing the death of brain tissue. Click on illustration to enlarge.
Image: National Institutes of Health
About 80 percent of all strokes are ischemic strokes. Blood clots in arteries are the most common cause. If an artery that supplies blood to the brain becomes clogged, the brain does not receive enough blood flow, and hence, enough oxygen. That leads to a brain infarction.
In an ischemic stroke, the blood supply to part of the brain is cut off. There are different ways the blood supply is blocked, include the most common:

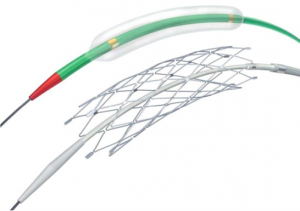
Recanalization is a possible treatment for ischemic stroke. Devices, such as Solitaire (top left), Penumbra (top right), and Trevo (bottom), are used to retrieve and/or aspirate the clot directly out of the artery and reopen the blocked blood vessel.
Blood clots can travel to the brain from another artery or from the heart. It is important to keep in mind other conditions can make a person vulnerable to a stroke, such as dehydration, illness and conditions that cause a hypercoaguable state, and low blood pressure.
Another possible source for stroke is a carotid or vertebral artery dissection. An injury to the blood vessel wall will result in potential blood vessel occlusion or formation of blood clots. The injury to the blood vessel can happen spontaneously or as a result of hyper rotation, flexion or extension of the neck. Not infrequently neck pain is associated with TIA-like symptoms.
Ischemic stroke can be caused by a blockage anywhere along the arteries feeding the brain. The blockages can occur for many reasons, including:
Strokes may also cause swelling in the brain. The pressure from this swelling can cause damage to brain tissue creating worse neurological problems.
Risk factors for ischemic stroke include:
Most strokes happen suddenly and damage the brain within minutes. In rarer cases, a stroke may get worse for several hours up to a day or two as a steadily enlarging area of the brain dies. This is called “a stroke in evolution.„
The common symptoms of ischemic stroke include:
A stroke is diagnosed by clinical exam and history and confirmed with CT and/or MRI imaging.
The treatment of ischemic stroke depends on how soon a person can get to the hospital after the onset of symptoms AND other medical conditions they may have.
If a stroke victim arrives at the hospital within 4.5 hours of the onset of symptoms, they may be eligible for a blood thinning medication to break up the clot in the arteries, called tissue plasminogen activator (tPA). However, this drug is only successful if patients receive this medication within the first 4.5 hours of onset of stroke symptoms. Fewer than 5 percent of stroke sufferers in the United States receive tPA because they do not get to the hospital fast enough to be offered treatment. Of those who are eligible, only about 30 percent of patients have improved symptoms after tPA administration; for the others, the clot is too big for tPA to breakdown.
A mechanical thrombectomy that aims to mechanically retrieve and/or aspirate the clot directly out of the artery via an angiogram procedure may be an option. This procedure is often used in conjunction with IV tPA administration and/or if IV tPA has been unsuccessful in reopening the blocked blood vessel. It involves the use of stent retriever devices and/or aspiration systems to pull the clot out of the blood vessel, reopen the blocked vessel and reestablish normal blood flow to the brain.
A mechanical thrombectomy can be offered up to 8 hours post stroke onset. In certain cases, it can be offered beyond 8 hours of onset.
It is important to understand: TIME IS BRAIN. The sooner blood flow resumes, the less chance brain cells will continue to die.
Ultimately, the best treatment against stroke is prevention.
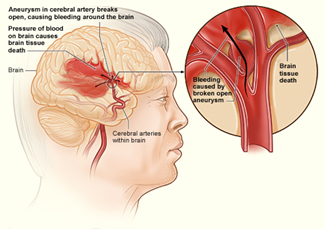
The illustration shows how a hemorrhagic stroke can occur in the brain. An aneurysm in a cerebral artery breaks open, which causes bleeding in the brain. The pressure of the blood causes the death of brain tissue. Click on illustration to enlarge.
Image: National Institutes of Health
A brain bleed is the type of stroke known as hemorrhagic stroke. It occurs when a blood vessel breaks or ruptures causing bleeding into the brain and killing brain cells. This type of stroke accounts for about 20 percent of all strokes. Hemorrhagic stroke often occurs due to long-term high blood pressure. Bleed from this type of stroke can occur:
There are two types of hemorrhagic strokes:
These include:
Signs of bleeding inside the skull tend to come on rapidly and include:
Description of the symptoms will typically lead a doctor to suspect a brain bleed and order a series of tests, which can include:
Treatment for bleeding inside the head varies on type of bleed, location and size—and may include:
Scientific Information courtesy of Demetrius Lopes, MD., Rush University Medical Center.